Why Kegels May Not Be the Best Choice for Most Women with Pelvic Floor Dysfunction
When we hear “pelvic floor dysfunction,” the first thing that often comes to mind is the classic advice:
“Do your Kegels!”
But here’s the truth...
Kegels are not a one-size-fits-all solution. In fact, for many women—especially those experiencing symptoms like leaking, prolapse, pelvic pain, or a constant feeling of pressure or tension—Kegels may not help at all.
They could even make things worse.
Let’s break down why that is.
1. It’s Not Always About Weakness
Kegels focus on tightening (contracting) the pelvic floor muscles. But what if those muscles are already tight or overactive?
Many pelvic floor issues aren’t caused by weakness—they're caused by a lack of relaxation, chronic gripping, or compensations from imbalances elsewhere in the body. In these cases, adding more tension through Kegels is like trying to fix a clenched fist by squeezing it even harder.
More contraction is not the answer.
2. You Need Coordination, Not Just Strength
Your pelvic floor isn’t meant to work in isolation—it’s part of a complex, coordinated team. It works alongside your diaphragm, deep core, hips, feet, and nervous system.
What your body really needs is a responsive pelvic floor:
One that contracts when needed, relaxes when it’s safe, and moves rhythmically with your breath and posture.
Kegels isolate the pelvic floor from this team. They often fail to restore true function—and can even create further imbalance.
3. Many Women Aren’t Doing Them Correctly
Even with instruction, studies show that many women don’t perform Kegels effectively.
They might:
Squeeze their glutes or thighs
Bear down instead of lifting
Hold their breath or increase intra-abdominal pressure
Without proper guidance and body awareness, Kegels can end up reinforcing the exact patterns that contributed to the dysfunction in the first place.
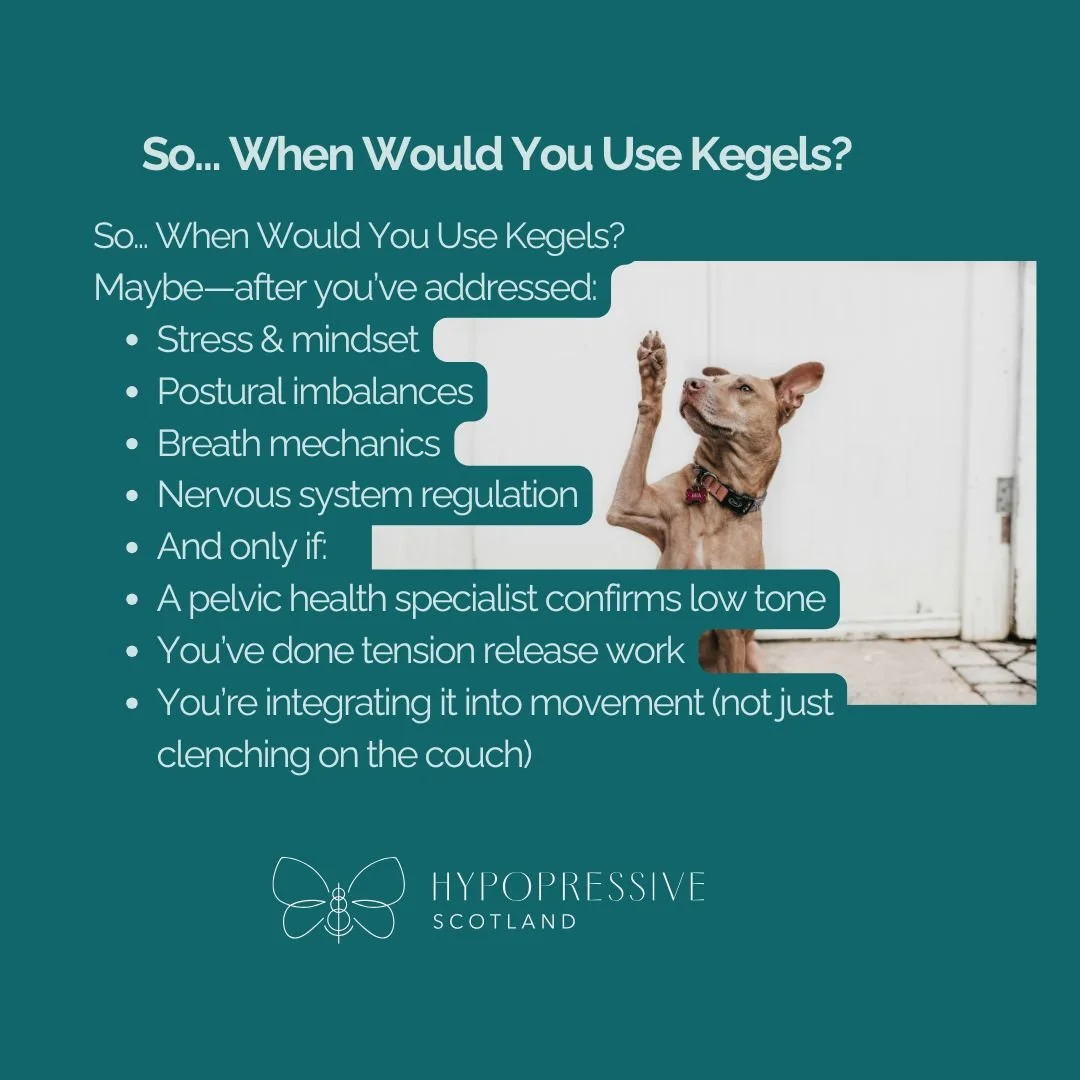
So… When Would You Use Kegels?
Kegels can perhaps be helpful once you’ve already addressed the foundations—like stress, posture, tension patterns, and breathing imbalances.
And only then, under specific conditions:
A pelvic health specialist has assessed and confirmed you have low tone or poor voluntary control
You’ve done the necessary downtraining and nervous system regulation work
You’re integrating the contraction into functional movement, not doing hundreds of squeezes in isolation
But even then... Kegels aren’t the whole solution.
The Bigger Picture: Why Kegels Alone Fall Short
Even if you’ve downtrained or know you have low tone, Kegels still don’t address the whole of you.
If your:
Posture is collapsed or tense
Breath is shallow or disconnected
Nervous system is on high alert
...then adding Kegels on top of that can disrupt rather than support healing.
In movement—like squatting, lifting, or walking—Kegels can interfere with your body’s natural patterns.
If you Kegel during a squat, for instance, you might:
Trap pressure downward onto the pelvic organs
Prevent the pelvic floor from rebounding naturally
Cause a “bum tuck” or posterior tilt, interfering with healthy load transfer
This creates a cycle of tension rather than the flow and support your body needs.
A Better Way Forward
What if, instead of gripping harder…
You restored your breath?
Supported your nervous system?
Reclaimed your body’s natural movement patterns?
Then, if Kegels have a role, it’s as a small part of a much larger, more integrated picture.
Where Holistic Therapies Shine
This is where approaches like Hypopressives and functional movement based on biomechanics really shine.
These therapies:
Encourage decompression and lift pressure away from the pelvic floor
Teach your body to self-regulate intra-abdominal pressure
Support posture, breath mechanics, and reflexive core activation
Involve your whole system—not just one isolated group of muscles
Hypopressives especially offer a gentle, effective way to:
Improve pelvic organ support
Reduce prolapse symptoms
Rewire the breath-pelvic floor connection
Help you feel lifted, stable, and empowered
Healing Is a Whole-Body Process
Healing isn’t about doing more.
It’s about doing what makes sense for your body, in the right sequence, with the whole system in mind.
And yes—it does take time.
My Personal Take
Yes, I still do a Kegel or two now and then.
Not because I need to fix anything—but because I like to check in.
To confirm that all the work I’ve done—Hypopressives, mindset shifts, nervous system work, and functional training—has given me a pelvic floor that’s responsive, not reactive.
I can squeeze if I want to.
And that’s powerful.
One Final Thought
I know it can feel scary to ignore what your pelvic floor physio told you.
But pause and reflect…
Did they ever ask you about:
How you breathe?
Where you hold tension?
Your nervous system state?
Your everyday posture or movement habits?
Or did they assess just one part of the team?
You are more than a pelvic floor.
You are a whole system.
And healing starts with honoring the whole of you.
If you’re ready to explore Hypopressives or take a whole-body approach to pelvic healing, let’s talk.
💬 DM me
📅 Book a free clarity call
🌐 Learn more at: www.hypopressivescotland.com