How to Tell if Your Pelvic Floor Is Tight or Weak
Confused About Your Pelvic Floor? You’re Not Alone
If you’ve ever been told to “just do your Kegels,” you’re not alone.
Many women believe squeezing the pelvic floor tighter will fix leaking, heaviness, or pain. But here’s the truth:
👉 A pelvic floor can be tight and still weak
👉 Tightness and weakness can share the same symptoms
👉 And Kegels aren’t the answer for everyone
So how do you know what your body needs?
This guide will help you understand the difference, gently and clearly, so you can start to move forward with confidence.
Why “Just Do Your Kegels” Isn’t Always the Answer
The pelvic floor is part of a much bigger system including your breath, your posture, your deep core, and your nervous system.
When the pelvic floor is tight and already doing too much?
➡️ More squeezing can make leaking and pain worse.
When there’s true under-support?
➡️ Strength can help — but only once the body can release and relax first.
Your pelvic floor deserves coordination and balance, not more tension.
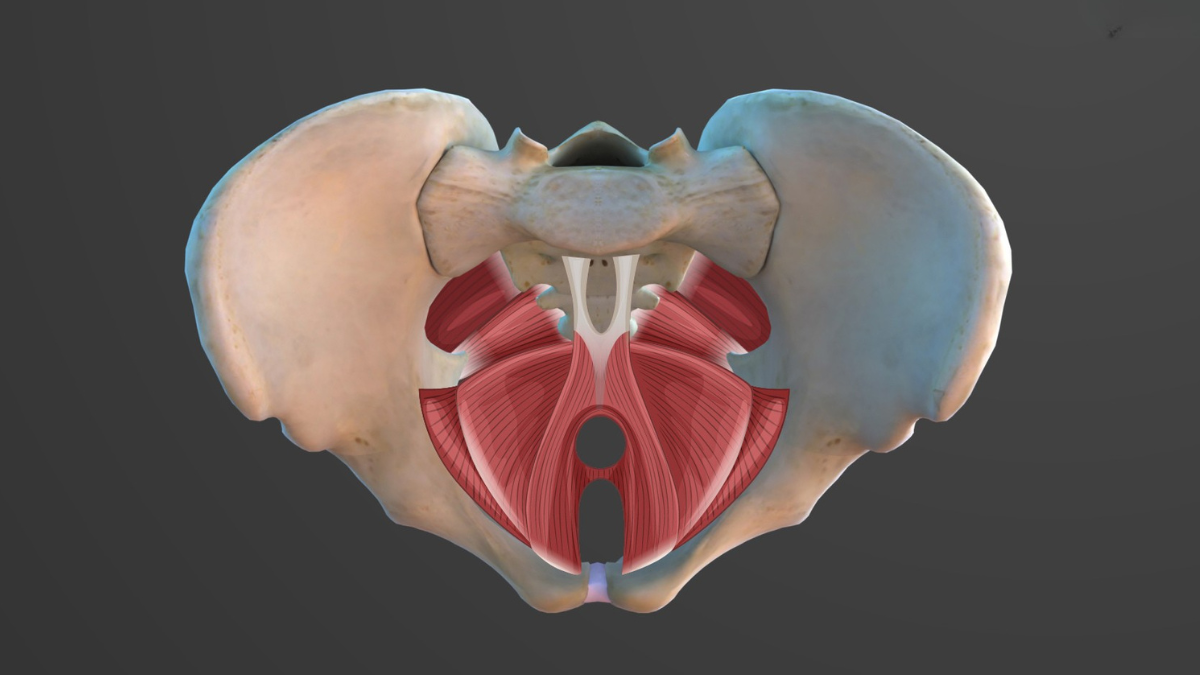
How This Small Group of Muscles Affects Your Whole Body
Your pelvic floor:
Supports bladder, bowel, and uterus
Helps control continence
Works with your diaphragm and breath
Stabilises your spine and hips
Responds to stress, pain, and emotion
Contributes to intimacy and pleasure
And to do all this well, your pelvic floor must be able to Contract, Release and Respond to your breath and movement.
Signs of a Tight Pelvic Floor
When “Holding On” Causes More Harm Than Help
You may notice:
Leaking with coughing, sneezing or running
Pain during sex or pelvic exams
Difficulty starting or finishing urine
Constipation or straining
Hip, lower back or tailbone tightness
A sense of clenching or gripping
This often comes from stress, trauma, birth recovery, or bracing habits.
This isn’t a failure.
It’s your body trying to protect you.
Signs of a Weak Pelvic Floor
When Support Is Missing
You may notice:
Heaviness or a dragging sensation
Leaking during movement, running or laughing
Difficulty holding wind
Visible bulge or prolapse symptoms
Reduced awareness or tone
This can follow childbirth, surgery, hormonal shifts, or long-term disconnection.
Most women have a combination:
Certain areas too tight. Others needing support.
Why Stress, Breath & Posture Matter
The pelvic floor responds directly to how safe the body feels, which is why approaches such as somatic therapy in Edinburgh and nervous system-led work can be so supportive for pelvic floor healing.
When the brain senses stress — emotional or physical — the body tightens:
Jaw clenches
Breath lifts
Ribs rise
Pelvic floor grips
“If your body feels unsafe, it holds on.
The goal isn’t to force strength —
it’s to create safety, so the body can restore it naturally.”
When breath expands with freedom, the pelvic floor can move with ease too.
The Pelvic Floor Diamond
Here’s a simple way to picture it:
Coccyx
Left sit bone
Right sit bone
Pubic bone
Together, they form the diamond of support — a shape that should gently draw together and release apart.
Simple Awareness Exercises
These are not tests — simply quiet check-ins:
Does your pelvic floor soften as you exhale?
Do your glutes clench without you noticing?
Is your jaw tense when symptoms increase?
Can your belly expand when you breathe?
Awareness is the first step in changing long-held patterns.
From Release to Strength — What Your Body Really Needs
This is where pelvic floor isolation exercises (often called “Kegels”) can be supportive — when done with lift, release, and timing.
A functional contraction:
1️⃣ Gently closes the openings
2️⃣ Lifts upward inside the body
3️⃣ Fully lets go afterward
Not clenching your bum.
Not breath-holding.
Not pushing down.
Try This: “Closing the Cathedral Doors”
Imagine your labia are cathedral doors
Close them softly
Allow the lift to travel upward — like a handkerchief or kite rising inside you
Release fully and wait for softness to return
Release is just as important as the lift.
When to Use Pelvic Floor Isolation Exercises
If your pelvic floor is… Tight
Start with… Breath + release + safety
Then progress to… Isolation exercises later
If your pelvic floor is… Weak
Start with… Gentle lift + awareness
Then progress to…Functional strength
If your pelvic floor is… Both
Start with… Nervous system + posture
Then progress to… Balanced release + strength
Every pelvic floor exercise has its place — when the body leads the timing.
Creating Long-Term Balance
Supportive recovery may include:
Breath-led movement
Hypopressives for pressure balance
Somatic release (TRE®, touch, grounding)
Posture and rib mobility
Strength that doesn’t create bracing
Working With a Pelvic Floor Specialist
If symptoms are persistent, a personalised assessment with a pelvic floor therapist can help you understand:
Where tension lives and why
Which muscles need more coordination
How breath and movement can support healing
How to rebuild confidence in daily movement
I’m Abby — a pelvic floor and nervous system specialist based in Edinburgh and working online.
You don’t need to figure this out alone.
👉 Explore Supported Functional Pelvic Floor
Strength Isn’t the Goal — Connection Is
Your pelvic floor isn’t broken.
It’s communicating.
When you learn to listen:
Breath returns.
Ease returns.
Confidence returns.
Strength follows connection.
Always.