The Femoral Cutaneous Nerve: The Overlooked Nerve That Can Mimic Pelvic, Hip & Thigh Pain
Pelvic tilts to release pain, bussing or numbness down the thigh
There’s a particular kind of discomfort I see again and again in women. It shows up as a burning, buzzing, numb or irritating sensation across the front or outer thigh.
It doesn’t behave like muscle pain. It doesn’t stretch out. And it doesn’t respond to strengthening.
Often, it’s not the hip… not the pelvic floor… not the lower back.
It’s a nerve.
And an often overlooked one at that, the femoral cutaneous nerve.
Let’s clear up the name (because it’s confusing)
When people talk about the femoral cutaneous nerve, they’re often referring to the lateral femoral cutaneous nerve, the sensory nerve involved in a condition called meralgia paraesthetica (“Meralgia” means, pain in the thigh, and “paresthetica” means, burning pain, tingling or itch.)
Important point: This nerve is sensory only. It does not control muscles.
So if someone is telling you to strengthen your way out of burning, numbness or pins-and-needles on the thigh… that should already raise a flag.
Where does this nerve come from?
The lateral femoral cutaneous nerve arises from the lumbar spine (L2–L3 nerve roots).
From there, it:
Travels through the pelvis
Passes close to the iliacus and psoas muscles
Runs under or through the inguinal ligament
Emerges near the ASIS (that sticky-out pelvic bone at the front, sometimes mistaken for your hip)
Supplies sensation to the outer and front thigh
The journey this nerve takes is important, because every one of those areas can influence how free (or irritated) this nerve feels.
What does irritation feel like?
Femoral cutaneous nerve irritation doesn’t feel like a pulled muscle.
Women often describe: Burning or heat across the thigh, tingling or pins and needles, numb patches, a buzzing or electric quality, pain that worsens with standing, walking or tight clothing
And crucially: It may ease when sitting or lying, stretching the thigh often doesn’t help, strength work can make it worse
Why this matters for pelvic floor health
This is where things get interesting.
Although the lateral femoral cutaneous nerve doesn’t innervate the pelvic floor directly, it shares:
Lumbar nerve roots
Fascial pathways
Pelvic and hip space
If the nervous system is overly sensitised, perhaps through stress, trauma, surgery, pregnancy, postural habits or chronic bracing, nerves stop gliding well. And when nerves don’t glide well, muscles often overprotect.
This overprotection might show up as a range of symtoms from: pelvic floor overactivity, hip flexor tension, rib gripping, breath-holding, anterior pelvic tilt or stiffness through the pelvis
The nerve irritation isn’t separate from the system it’s actually a part of it.
Common contributors I see
This nerve is particularly vulnerable to compression and tension, rather than injury.
Common contributors include:
Tight waistbands, shapewear or belts
Prolonged sitting
Pregnancy and postpartum changes
Scar tissue (C‑sections, abdominal or pelvic surgery)
Strong gripping through the lower abdominals
Overzealous core or hip flexor training
Nervous system up‑regulation and chronic stress
Sexual abuse
Notice how few of these are what we consider “weakness” problems.
Why traditional exercise often misses the mark
If a nerve is irritated, asking surrounding muscles to work harder rarely helps.
In fact, it often increases compression at:
The inguinal ligament
The front of the hip
The lumbar spine
This is why some women notice their symptoms appear after they start exercising “for their core” or “for their pelvic floor.” This is something I have noticed over the past decade - the order we introduce methods to our body system is very important.
A different approach, one that respects the nervous system
In my work, the starting point is never: “Let’s strengthen that.” It’s: “Can this system feel safe enough to let go?”
That might include:
Gentle nerve‑friendly movement, not aggressive stretching
Reducing abdominal gripping and pressure habits
Breath‑led work to calm the nervous system
Hypopressives used appropriately to rebalance pressure rather than force control
Pelvic and rib cage mobility
Scar tissue and fascial awareness
Sometimes TRE® or gentle shaking to reduce global tone
When the system settles, nerves often calm, without being targeted directly.
Simple release options for you to try now (gentle and nerve‑friendly)
These are not stretches and they’re not about forcing anything to change. Think softening, unloading and creating safety for the nervous system.
1) Inguinal ligament softening (hands & breath)
Why: This is the most common point of irritation for the lateral femoral cutaneous nerve, just below the ASIS, where it passes under the inguinal ligament.
How:
Lie on your back or sit comfortably
Place fingertips just inside and below the ASIS (front of pelvic bones)
Use very light pressure, this is not massage
Breathe slowly into the ribs for 60–90 seconds
On each exhale, imagine the tissue softening and widening
Cue:
“Less pressure than you think. This is listening, not digging.”
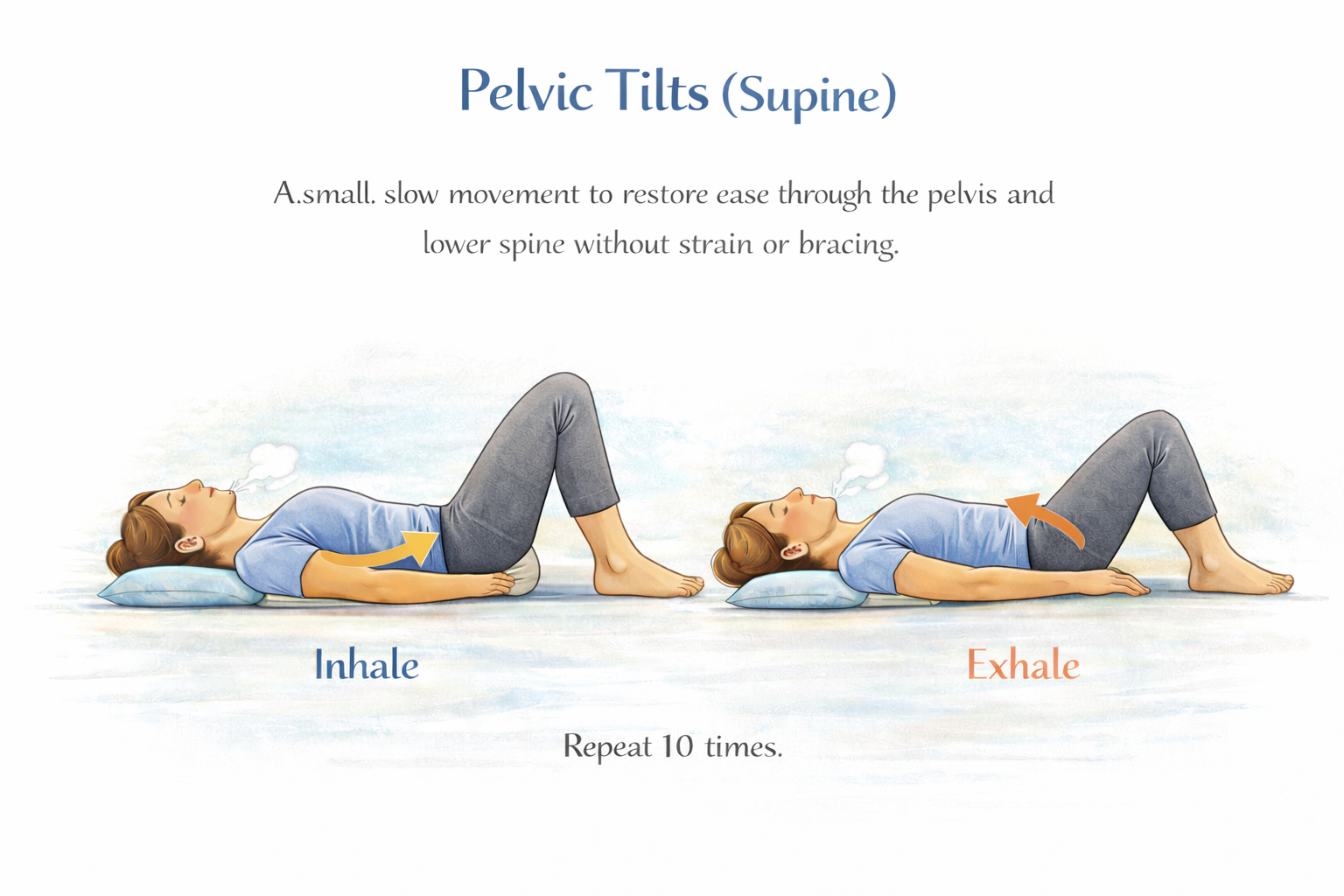
2) Pelvic rocking with long exhale
Why: This gently unloads the front of the hip, reduces tone through the iliacus and abdominal wall, and allows the nerve to glide without being stretched.
How:
Lie on your back with knees bent, feet on the floor
Inhale → a small anterior pelvic tilt
Long exhale → a gentle posterior pelvic tilt
Keep the movement slow and subtle
6–10 easy rounds
Cue:
“Let the breath lead the movement — not effort.”
30 Side‑lying hip unweighting
Why: Takes pressure off the inguinal region and front of the hip without pulling on the nerve.
How:
Lie on your non‑symptomatic side
Bottom leg bent, top leg supported on cushions
Let the top thigh feel heavy and fully supported
One hand on the ribs, one on the belly
Breathe slowly for 1–2 minutes
Cue:
“You’re not stretching, you’re letting the front of the hip stop holding.”
Important notes:
❌ Avoid aggressive hip flexor or quad stretches
❌ Avoid strong abdominal bracing
❌ Avoid foam rolling directly over the front of the hip
If symptoms increase, stop. Nerves calm with safety, not force. So, if we tell the body you are listening by stopping the next time you do it your nervous system will trust the process a little more.
A quiet reminder
If you’ve been told:
“Your scans are fine”
“Just strengthen your core”
“It’s probably your hip”
…but your symptoms feel nervy, change with stress, clothing or posture, and don’t behave like muscle pain, trust that information. Your body isn’t failing. It’s trying hard to communicate.
If this resonates
If you’re navigating unexplained thigh discomfort alongside pelvic floor symptoms, prolapse, bladder issues or persistent tension- this is work I do every day.
Not by chasing symptoms. But by helping the whole system reorganise. You don’t need more effort. You need the right order.
Want support?
If this feels familiar, thigh symptoms that don’t behave like muscle pain, pelvic floor tension that won’t settle, or a body that feels stuck in protection - you don’t need to figure it out alone.
This is exactly the kind of whole‑system work I support:
understanding why your body is holding
calming the nervous system first
then rebuilding coordination, breath and strength in the right order
You can work with me 1:1 personalised support is the best place to start.
Your body isn’t playing up or being difficult. It’s asking for a different conversation.
Book a session …